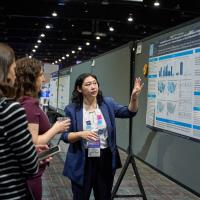
Alumna Spotlight: Josephine Nhu Tran
Originally published in the Sept. 2019 AMCP Foundation Insights e-newsletter.
Over the past 26 years, nearly 200 student pharmacists have taken part in our summer internships. We're pleased to highlight our intern alumni in this reoccurring feature.
Name: Josephine Nhu Tran, PharmD, MS
Current Title: Director of Outcomes-Based Contracting and Pharmacy Programs at UnitedHealthcare.
Internship Program: AMCP Foundation/Pfizer, Inc. Managed Care Internship
Internship Site: VA Long Beach
Year: 2007
Josephine Nhu Tran, PharmD, MS, is the Director of Outcomes-Based Contracting and Pharmacy Programs at UnitedHealthcare. She has been with UnitedHealth Group for over 7 years and in her prior roles in the organization, she served as Associate Director on the Optum Health Economics and Outcomes Research (HEOR) team and Associate Director of Clinical Outcomes Research at OptumRx. Prior to joining UnitedHealth Group, Josephine worked as a formulary manager at the Department of Veterans Affairs where she performed formulary operations and research to support the formulary decision making process. She earned her PharmD, MS in Pharmaceutical Economics and Policy, and Certificate of Gerontology from the University of Southern California. She also completed a post-doctoral HEOR fellowship with Amylin Pharmaceuticals in partnership with the University of Southern California.
What does a typical day look like?
One of the things I enjoy most about my job is there is no typical work day and I’m constantly working on new strategies and learning new things. In my role, I have the opportunity to develop innovative payment strategies with the goal of driving down total-costs-of-care for our clients and members. I work closely with internal stakeholders and manufacturers to develop “win-win” strategies for our organizations. Typical things that I work on include developing payment strategies (e.g., outcomes-based contracts), developing models to determine the value of these strategies, discussing these strategies with manufacturers, working with our internal Optum vendor on adjudicating outcomes-based contracts, and reporting the outcomes of these strategies to leadership. Since my team covers all therapeutic areas, we work closely with our clinical teams at UHC to understand the treatment landscape to develop these strategies. My team also develops pharmacoeconomic evaluations and outcomes analyses to support our Prescription Drug List (PDL) committee decisions.
What types of managed care practices do you use in your work?
As part of the pharmacy management strategy team, my team strives to manage medical and pharmacy drugs based on their total value to the health plan (e.g., total costs of care, pharmacoeconomic value) and do so using managed care practices such as formulary management and utilization management to drive utilization and care to the drugs with most value.
How did the Foundation Internship prepare you for your career?
The Foundation Internship was the driving force for my career in research and its applications in managed care. I was involved with the AMCP chapter at the University of Southern California (USC) where I served as chapter president. However, it was through the internship that I was inspired to use data to drive decision-making. I interned at the VA Long Beach where I had wonderful preceptors that allowed me the opportunity to conduct several real-world studies that would impact policy development - one examining whether clinical practice guidelines were being followed and the other examining the safety outcomes associated with drug treatments. It was this experience that paved the way for my interest in real world research, data, and its use in formulary and clinical practice decision making.
Anything else you’d like to add?
I have had the opportunity to work in different parts of the managed care arena from an HMO setting to a pharmacy benefit management company and to a health plan. I believe pharmacists are in the unique position at all levels to make population level impacts that will drive affordability and improve quality of care in the healthcare system.